Central Maine Healthcare Careers


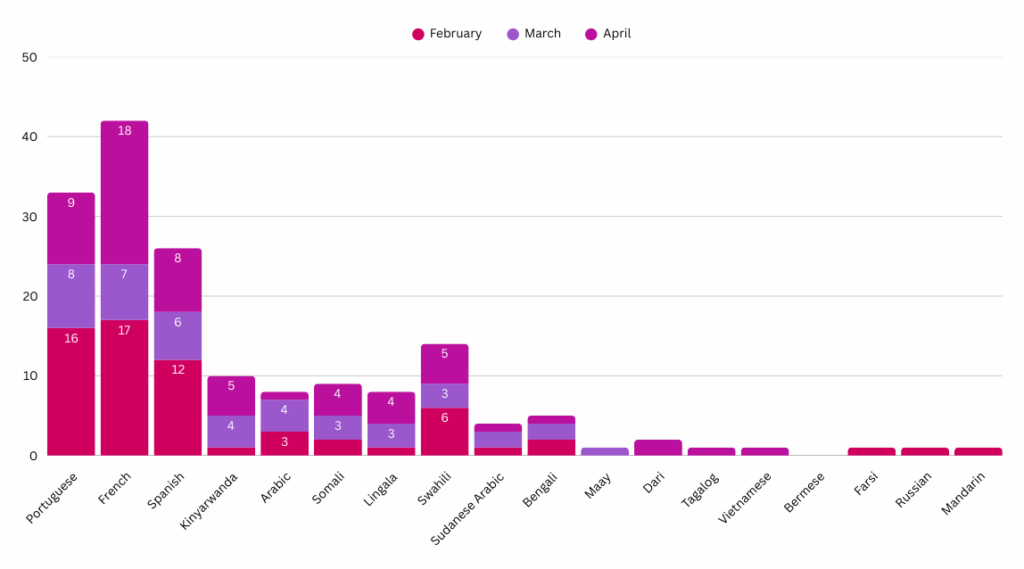
The following graph depicts the total number of calls received by our language assistance services program to overcome any patient/provider communication barriers. Our hope is to give insight to the diversity of languages spoken in our communities.






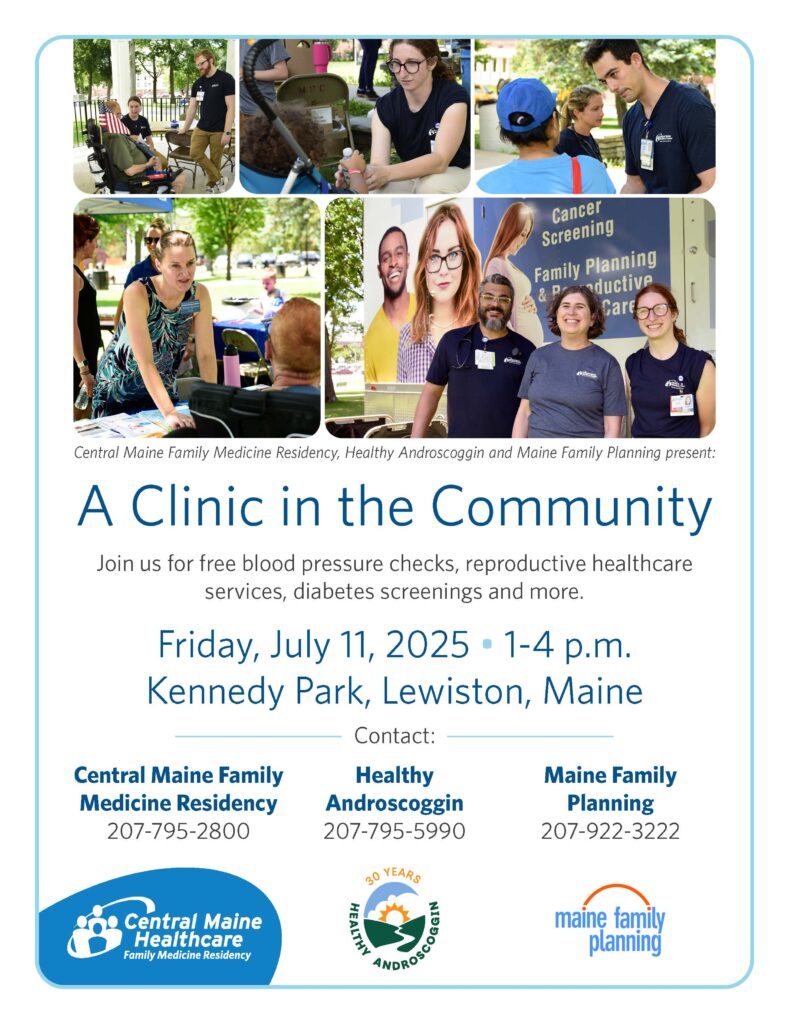
Photos from 2024’s Clinic in the Community

Central Maine Healthcare is an integrated healthcare delivery system that serves residents of central, western and midcoast Maine. Our close-knit teams provide exceptional care and innovative treatments, and we, in turn, invest in their professional growth and development. We offer opportunities for physicians, advanced practice providers, nurses, therapists, technicians, hospital administrators and anyone else looking to establish or advance a career in healthcare.





CMH offers a robust benefits package called that includes:
We offer paid time off and other measures to ensure a healthy work-life balance. Learn more…






While not at work, our team members enjoy the endless opportunities for entertainment that Maine has to offer. Outdoor enthusiasts can enjoy skiing, boating along the coast and hiking at a state or national park. Centrally located to several popular attractions, residents can embark on day trips to Boston, North Conway, New Hampshire and Boothbay Harbor. Maine is a wonderful place to raise a family, with safe communities and great public and private schools.
You can find a place here at CMH — no matter your specialty. We have both clinical and nonclinical positions available. Click on the link below for more information. Find more…
Mission: To train residents to competently triage, diagnose and treat a wide variety of medical concerns commonly seen in low resource settings which includes but is not limited to wilderness and international areas, while empowering residents with the tools to push their boundaries of knowledge when it comes to providing care in such settings.
Goal 1: Develop the ability to provide medical care performed in low resource and stressful situations with appropriate attention to detail (PROF 2).
Objectives:
Goal 2: Demonstrate an ability to optimize resources available in low resource situations (MK1, PC5).
Objectives:
Goal 3: Formulate a learning plan independently related to an area of low resource medicine that has special interest to you (PBL2).
Objectives:
Goal 4: Integrate knowledge obtained through clinical and didactic settings to maximize the chance of survival of self and party/patients under your care in a wilderness setting (MK1, PC5).
Objectives:
Goal 5: Perform basic improvised medical procedures and protocols with reasonable confidence and motor skills when in low resourced settings (PC5).
Objectives:
Goal 6: Be prepared to give recommendations for patients who will be in situations where they will not have access to the resources of CMMC or similar hospital (PC3).
Objectives:
Goal 7: Develop illness scripts for common causes of morbidity and mortality in low resource settings (PC1).
Objectives:
Using WIMP Funds: After using WIMP funds, the resident will be required to do a presentation on their trip/learning. If WIMP funds are used for an Away-away rotation, that doesn’t mean CME funding for that rotation is approved as well. That would also require approval from the PD. If you get approval to also use CME funding, the expectation is within 3 months of returning, you do a presentation that includes a review of the literature and evidence for an intervention or problem addressed, you saw on the trip. Those presentations should be reviewed by Dr. Pomeranz at least 1 week prior to the scheduled date. The program coordinator or scheduling coordinator can help you find a time to present either within the didactic calendar or a non-Tuesday.
Ice Fishing 2025



2024 FMEC

2024 FMEC






 Pruthvi Kilaru, DO, MPH He/Him/His Meet Dr. Kilaru Pruthvi.Kilaru@cmhc.org |  Jacob Lamoreau, MD He/Him/His Meet Dr. Lamoreau Jacob.Lamoreau@cmhc.org |  Audrey Micallef, MD She/Her/Hers Meet Dr. Micallef Audrey.Micallef@cmhc.org |
 Isaac Peacock, DO Meet Dr. Peacock Isaac.Peacock@cmhc.org  Amer Zia, MD Meet Dr. Zia amer.zia@cmhc.org |  Will St. Marie, DO He/Him/His Meet Dr. St. Marie William.StMarie@cmhc.org |  Berna Urkmez, MD She/Her/Hers Meet Dr. Urkmez Berna.Urkmez@cmhc.org |
Class of 2027
 Jesse Atwood, DO He/Him jesse.atwood@cmhc.org |  Christine Nwoke, DO christine.knowe@cmhc.org |  Sydney Morse, MD She/Her/Hers Meet Dr. Morse sydney.morse@cmhc.org |
 Sarah Nasrallah, MD She/Her Meet Dr. Nasrallah sarah.nasrallah@cmhc.org |  Al Privorozky, MBB Ch He/Him Meet Dr. Privorozky al.privorozky@cmhc.org |  Sarah Sacco, DO She/Her Meet Dr. Sacco sarah.sacco@cmhc.org |
 Kevin Stavness, DO He/Him Meet Dr. Stavness kevin.stavness@cmhc.org |
 Alexander Babaoghli, DO Alexander Babaoghli, DOCo-Chief He/Him/His Meet Dr. Babaoghli alex.babaoghli@cmhc.org |  Ramneek Gill, MD Meet Dr. Gill ramneek.gill@cmhc.org |  Sarang Kumar, MD Meet Dr. Kumar sumar.kumar@cmhc.org |
 Dillon Lawler, DO Co-Chief He/Him Meet Dr. Lawler dillion.lawler@cmhc.org |  Amy Mack, MD She/Her Meet Dr. Mack amy.mack@cmhc.org |  Robyn Rowell, DO Meet Dr. Rowell robyn.rowell@cmhc.org |

Patricia (Patty) Collins, D.O., OMM (She/Her/Hers) Interim Program Director
Faculty
collinpa1@cmhc.org
Medical School: University of New England College of Osteopathic Medicine
Residency: Central Maine Medical Center Family Medicine Residency
After completing my residency and serving as chief resident at CMMC, I was excited to be staying on as faculty. The culture at the residency was one that strives towards growth and commitment to quality education and patient care. Being a faculty member has allowed me to continue to practice medicine across both the outpatient and inpatient settings while incorporating my passion for medical education and teaching. I love working alongside residents and medical students, I find myself not only teaching but learning from our learners. It is a privilege to be a part of their individual growth as physicians.
Outside of work, I enjoy spending time outdoors. My husband and I love to take our daughter and dog hiking. I also enjoy biking, cooking, and attempting to garden.
Clinical Areas of Interest:
Inpatient Medicine
Family Planning
Breastfeeding Medicine
Scholarly Work:
Optimizing Graduate Medical Education during Early Residency
Society of Teachers of Family Medicine Residency Faculty Fundamentals Certificate

Annie Derthick, Ph.D. (She/Her)
Associate Academic Program Director
Director, Behavioral Science
Faculty
derthian@cmhc.org
Graduate School: University of Alaska
Area of Study: Clinical Community Psychology with a Rural and Indigenous emphasis
I fell in love with resident education when I completed my own clinical training in a residency clinic. There is no better place to do the work I want to do, which is to be engaged with the community to solve the problems that matter most. Primary care is the hub of community health and wellbeing in so many underserved communities, and residency clinics are perfectly situated to partner with patients, families, and communities to create innovative, lasting change. I consider it a privilege to educate family medicine residents. I love being a part of the journey of residents consolidating their identity as a family physician and agent of change in their community. My favorite moment is somewhere in the middle of third year when the picture finally comes into focus, and this learner, who I’ve been watching grow over the last couple of years, takes shape as the physician they were meant to be. They are confident, grounded, and ready to make a difference.
Outside of work, my absolute favorite thing in the entire world is my 7-year-old goldendoodle, Moxie. I have a 1-year-old poodle, Cricket, who is worming her way into my heart as well. I like to spend time with them, and my partner, Kris, outside in our backyard, especially in the fall. I love to read. And I love to laugh. Feel free to stop by any time if you have a good story to tell or want to hear one.
Clinical Areas of Interest: Integrated Behavioral Health, Supervision and Mentorship. Psychological Assessment, Motivational Interviewing, Health Behavior Change, and Structural Racism as a Social Determinant of Health.
Scholarly Work:
DISSERTATION
Derthick. A. O. The Sexist MESS: Development and initial validation of the Sexist Microaggressions Experiences and Stress Scale and the relationship of sexist microaggressions and women’s mental health (Doctoral dissertation). ProQuest Dissertations and Theses Global (No. 3470179).
BOOKS
David, E. J. R., & Derthick, A. O. (2017). The psychology of oppression. New York, NY: Sage.
PEER-REVIEWED JOURNAL ARTICLES
Brown, S. R., Friedman, R., McDermott, S., Oliveri, M., Derthick, A. O., & Picker, B. (2021). Highlights of the innovation showcase. Annals of Family Medicine, 19(4), 375-376. PMID#34264849

Genesis Juat, MD, Medical Director
I have a deep-seated belief that everyone should have access to healthcare—it’s a right, not a privilege. And having primary care as the heart of it all is vital for keeping our communities healthy and thriving.
My own curiosity has taken me on a journey through a variety of healthcare settings, from Federally Qualified Health Centers (FQHCs) as far west as Seattle to rural clinics in Maine, and eventually into leadership roles in hospital systems. These experiences have given me a broad perspective and allowed me to keep my practice diverse and dynamic. Moving into resident education felt like a natural step, sharing my experiences, and learning together as we adapt to the ever-changing world of medicine.
My interests include dermatology within primary care, behavioral health integration, international medicine, substance use disorder treatment, and the exciting ways technology enhances our practice. Yet, despite all the tech advancements, I still have a soft spot for my trusty old stethoscope from med school—it’s been with me through thick and thin.
My spouse is a local Mainer, and together we have 2 strong-willed kids and 2 Seattleite golden retrievers who have made an impressive transition from the urban sidewalks of Seattle to enjoying the open fields and cold Atlantic waters of Maine.
Medical School: A.U.A. College of Medicine
Residency: Central Maine Medical Center Family Medicine Residency

Chris Decker, D.O., OMM, DAAMA, DABOIM (He/Him)
Director of Integrative Medicine
Faculty
deckerch1@cmhc.org
Medical School: Touro University California
Residency: Central Maine Medical Center Family Medicine Residency
Fellowship: Integrative Medicine University of Arizona/ Maine Medical Center
I love being in an environment of active learners as it keeps me engaged, up to date, and provides unique perspectives that I don’t think I would be as exposed to otherwise.
There is an excitement and zest that I find energizing and motivating.
As faculty, I like to stress both the technical side of being a doctor but more importantly the healer/ humanistic side to build therapeutic relationships and individually tailored plans based on a person’s cultural background and personal values.
Outside of medicine, I enjoy being active whether it being playing soccer, frisbee or going on a hike and spending time with my wife, son, and dog.
Clinical Areas of Interest: Addiction, Integrative, Acupuncture, Homeless Youth
Scholarly Work:
Review of Effectiveness of Psilocybin for Depression. Integrative Medicine. 2022
Integrative Approach to Long Covid Seminar at Family Medicine Education Consortium. 2022
Creator and instructor for Intro to Integrative Medicine Course at Maine College of Healthcare Professionals 2021

Thomas Hattan, M.D.
Board Certified Palliative Care Medicine
Faculty
hattanth@cmhc.org
Medical School: Saint Louis University School of Medicine
Residency: Madigan Army Medical Center, Internal Medicine
Fellowship: Geriatrics, VA Madigan Army Medical Center
At the age of twelve I decided that I would be a Doctor and not a history teacher; thankfully my career has allowed me to create a medical practice but also share the joys of teaching. I have worked with the community of Lewiston/Auburn and the family medicine residency to provide care for in area Nursing Homes and Assisted Livings. Sharing that work living space with teammates, medical students, residents, nurse practitioners, and colleagues: I am proud of the home-based collaborative care we provide. In my work with medical learners, I strive to provide a community-based perspective that stresses the natural processes of the life, aging, and dying; how medicine can interfere and aid in these processes.
Teaching, learning, growing, the open exchange of ideas and practice: working with a Geriatric Team to provide as safe and comfortable place as we can is a rich challenge.
I live with my wife Robin and three dogs in Yarmouth, Maine. Three adult children enrich our world with adventures and growth. Seasons, travel, walks, gardening, sitting by the fire with a novel, I am proud and blessed with Yarmouth’s warm comfort.
Clinical Areas of Interest: Geriatrics and Palliative Care medicine and teaching. Helping medical learners understand the necessity of self, their individual perspective and voice as it impacts their practice of medicine. Understand and improve my own practice and team skill set. Build a Geriatric Team at the Family Medicine Residency.
Scholarly Work: My practice is that of a clinical provider. I am proud that five medical learners that I have shared my practice with have furthered their Geriatric and Palliative Care practice and education and of all the students and graduates that enrich our community.

Hannah Kazal MD, ScM (She/Her/Hers)
Faculty
Hannah.Kazal@cmhc.org
Fellowship: Addiction Medicine Fellowship, Maine Medical Center
Residency: Sutter Santa Rosa–UCSF Family Medicine Residency
Medical School: Warren Alpert Medical School of Brown University
Dual degree: M.D., Sc.M. (Master of Science in Population Medicine)
She graduated from Brown University Medical School with dual MD and Master of Science in Population Medicine degrees. Residency pulled her to the West Coast, where she graduated from Sutter Santa Rosa-UCSF Family Medicine Residency as an HIV specialist and CREATE (Continuing Reproductive Education for Advanced Training Efficacy) trainee with advanced reproductive health skills. Through residency as a third-year running the inpatient medicine, obstetrical, and outpatient services, she discovered her enthusiasm for medical education and decided to pursue an academic fellowship in Addiction Medicine.
Clinical Areas of Interest: She is passionate about dismantling health inequities and expanding access for marginalized populations such as those living with SUDs, HIV, unhoused communities, and carceral histories. She is an advocate for the integration of harm reduction into clinical care and enjoys providing education on this evidence-based practice to colleagues, medical trainees, and patients. As a Family Physician, Dr. Kazal maintains a broad practice in comprehensive reproductive health, HIV/HCV prevention/treatment, and procedures with general primary care of patients and families through peripartum, childhood, and aging, from the acute hospital to community settings.
CMMC Family Medicine Residency
76 High Street
Lewiston, ME 04240
Tel. 207-795-2184
Fax. 207-795-2190

Lauren Nadkarni, M.D., CAQSM, FAAFP(She/Her/Hers)
Assistant Regional Dean, UNECOM
Director of Undergraduate Medical Education
Medical School: Tufts University School of Medicine
Residency: Maine Medical Center, Portland, ME
Fellowship: Sports Medicine, Maine Medical Center, Portland, ME
I have been working in medical education and as Family Medicine residency faculty for the past 7 years and have been the Regional Assistant Dean of Education at UNECOM since 2022. In my role as Undergraduate Medical Director, I enjoy working with learners from a variety of backgrounds and with diverse experiences as they learn from and contribute to our educational environment at CMHC. Clinically, I believe in promoting health and supporting preventative care efforts through physical activity based on the belief that ‘exercise is medicine’ and I work with patients using shared decision-making to provide creative solutions to their unique healthcare needs. While my clinical interests are sports medicine, Point-of-Care Ultrasound (POCUS), and collegiate health, I enjoy incorporating learners into these varied clinical environments and sharing the breadth of Family Medicine with them. When I’m not working, I enjoy traveling and being active outdoors, hiking, playing sports, tending my vegetable garden, and spending time with my family and my dogs.
Clinical and Educational Experiences
We foster a collaborative environment centered on Central Maine Healthcare’s tradition of excellent medical education while anticipating the changing needs of our community. We strive to cultivate compassionate, socially responsible leaders who create the future of healthcare for all.
Our residency is a host Core Clerkship site for the entire third year of clinical experiences for the University of New England College of Osteopathic Medicine (UNECOM). We accept a total of twelve students from UNECOM, who are matched to our site through a lottery process.
We are also a core site for 3rd-year Family Medicine Clerkships at Tufts University (Maine Medical) School of Medicine and the Larner College of Medicine at the University of Vermont.
We strive to provide an optimal learning experience by allowing students to be involved in all aspects of medical education. We will only schedule rotations when there is no conflict with resident education. Rotations are also available to students from other U.S., Canadian, and international medical schools.
What We Offer to Students
· CMMC is located within walking distance to many restaurants, shops, services, and places of worship. It is also close to Bates College. · Transportation services are easily accessed.
· In Lewiston, apartment-style housing is provided based on availability, and priority is given to early applicants. It may be necessary for you to share a coed apartment if the student census is high. Apartments have a fully- equipped kitchen, provided linens, laundry on site, and wireless internet. No pets are allowed.
· Parking – Off-street parking is available to all students.
· Food – We are unable to provide free meals to elective students.
· For further questions please contact Katherine Truitt, Student Coordinator at Katherine.Truitt@cmhc.org or call 207-795-2824
Elective Clerkships
The following elective clerkships are available at CMMC and are coordinated by the Family Medicine Residency office. We only approve rotations that offer the best educational opportunities and clerkships are only scheduled when they will not conflict with resident education. We offer these rotations to students from U.S., Canadian and offshore medical schools. Our medical student education offerings are highly competitive, and our calendar fills up quickly. We accept students with quality applications and on a first come, first serve basis. Please apply as early as you can for a chance at a clerkship placement.
Family Medicine (Sub-Internship)
· 4-week clerkship
· Combination of Inpatient and Outpatient experience
· Opportunity for an evening call and weekend on-call shift
· Didactic sessions weekly
· Participate as a member of the patient care team
We offer other rotations on a case-by-case basis. Possible specialties include:
· Emergency Medicine
· Obstetrics and Gynecology
· Pediatrics
· Surgery
· Internal Medicine
· Rural Family Medicine
If there is a rotation you are interested in and do not see it listed, feel free to contact us to determine if it can be arranged. Even if a specialty is available, your desired dates may not be available. Our medical education program is extremely competitive, and we fill the available slots in our academic calendar based on the quality of application and on a first come, first serve basis.
If you have questions regarding a clerkship, contact Katherine Truitt, Student Coordinator at Katherine.Truitt@cmhc.org or call 207-795-2824.
Application Forms and Materials (click here)
Application materials in addition to the completed form
· Cover letter
· Curriculum vitae or resume
· Unofficial copy of your current transcript or similar record of academic performance
· United States Medical Licensing Examination Step scores or Comprehensive Osteopathic Medical Licensing Examination results (whichever is most recent/applicable)
If you have difficulty using the Smartsheet application form, please contact Katherine Truitt, Student Coordinator at Katherine.Truitt@cmhc.org
Documentation Requirements (Once Approved for a Rotation)
· Clinical Experience Agreement between your school and Central Maine Healthcare (Central Maine Healthcare will create a CEA with your school, if one is not already established.)
· Letter of Good Standing from your medical school
· Immunization Records for Measles, Mumps, Rubella, Hepatitis B, Varicella, Influenza (current season or most recent), and Covid-19 (most recent booster)
· A negative Tuberculin Test within 12 months of your approved rotation start date
-Professional Liability Insurance
· National Background Check is complete with satisfactory results. Local background checks are not accepted, and the results must include the following traces/searches
o Social Security Address/Alias trace
o State of Residence Criminal Background search
o National Sex Offender search
o Office of Inspector General search
o Excluded Party List System search
These documents are required after your application has been approved and you have a scheduled rotation start date.

