Mission: To train residents to competently triage, diagnose and treat a wide variety of medical concerns commonly seen in low resource settings which includes but is not limited to wilderness and international areas, while empowering residents with the tools to push their boundaries of knowledge when it comes to providing care in such settings.
Goal 1: Develop the ability to provide medical care performed in low resource and stressful situations with appropriate attention to detail (PROF 2).
Objectives:
- Identify barriers to providing quality medical care in resource-limited environments, including situations and stressors unique to these circumstances
- Develop strategies for overcoming the unique challenges of practicing medicine in resource-limited environments
- Appraise how those strategies worked and adjust them as needed
Goal 2: Demonstrate an ability to optimize resources available in low resource situations (MK1, PC5).
Objectives:
- Demonstrate summative knowledge of subsistence survival and natural resources (e.g., knowledge of edible plants).
- Classify different types of resources (such as consumable goods, non-consumable goods, individuals, knowledge, etc…)
- Execute utilizing available resources in different ways and an ability to generate new resources.
Goal 3: Formulate a learning plan independently related to an area of low resource medicine that has special interest to you (PBL2).
Objectives:
- List three knowledge areas related to WIMP you want to learn more about.
- Present to the residency in didactics on one of those areas after independently researching the topic.
- Reach out to others who have interests in those areas outside of our program.
Goal 4: Integrate knowledge obtained through clinical and didactic settings to maximize the chance of survival of self and party/patients under your care in a wilderness setting (MK1, PC5).
Objectives:
- Exhibit during stimulations the proper priorities of survival (for instance lack of shelter in an extreme environment is usually going to kill someone faster than lack of food).
- Implement learned skills to ensure survival needs are met (for example how to build a fire to keep warm in a cold setting).
- Use different tools at your disposal to communicate in these austere settings (such as taking advantage of sound, light, and other mediums to signal one is lost).
Goal 5: Perform basic improvised medical procedures and protocols with reasonable confidence and motor skills when in low resourced settings (PC5).
Objectives:
- Select whatever resources are available to evaluate the patient as thoroughly as possible (for instance improvising a stethoscope or blood pressure cuff).
- Demonstrate competency in performing procedures such as trauma care, wound care, pain management, airway management, etc… in low resource settings.
- Solve the best way to transport a patient in low resource settings (carries, litters, rescue sled, etc…)
Goal 6: Be prepared to give recommendations for patients who will be in situations where they will not have access to the resources of CMMC or similar hospital (PC3).
Objectives:
- Describe how you would do a comprehensive pretravel visit for a patient (including but not limited to which vaccines and prophylactic medication they should receive).
- Assemble a travel first aid kit for different environments.
- List other considerations for preparedness (clothing, food, etc…)
Goal 7: Develop illness scripts for common causes of morbidity and mortality in low resource settings (PC1).
Objectives:
- This includes but is not limited to altitude illnesses, marine/diving injuries, hot/cold as well as other weather-related pathologies, trauma (including mental), flora/fauna afflictions, and international infectious diseases while for each cause know prevention, diagnosis, and treatment.
WIMP Funding
Using WIMP Funds: After using WIMP funds, the resident will be required to do a presentation on their trip/learning. If WIMP funds are used for an Away-away rotation, that doesn’t mean CME funding for that rotation is approved as well. That would also require approval from the PD. If you get approval to also use CME funding, the expectation is within 3 months of returning, you do a presentation that includes a review of the literature and evidence for an intervention or problem addressed, you saw on the trip. Those presentations should be reviewed by Dr. Pomeranz at least 1 week prior to the scheduled date. The program coordinator or scheduling coordinator can help you find a time to present either within the didactic calendar or a non-Tuesday.
Resources
- Cushing TA, Harris NS, Auerbach PS. Auerbach’s Wilderness Medicine. Elsevier; 2017.
- Binder WD, ed. Wilderness & Environmental Medicine.
- CDC yellow book 2024. Centers for Disease Control and Prevention. August 14, 2023. Accessed March 21, 2024. https://wwwnc.cdc.gov/travel/page/yellowbook-home.
- Otten E, Bowman W, Hackett P, Spadafora M, Tauber D. Wilderness Prehospital Emergency Care (WPHEC) curriculum. Journal of Wilderness Medicine. 1991;2(2):80-87. doi:10.1580/0953-9859-2.2.80
- Pocket book of hospital care for children: Second edition. World Health Organization. Accessed March 21, 2024. https://www.who.int/publications/i/item/978-92-4-154837-3.
- Wild Med U. Accessed March 21, 2024. https://www.awls.online/podcasts.
- Mobile apps & Voice-Enabled Skills. Red Cross. Accessed March 19, 2024. https://www.redcross.org/get-help/how-to-prepare-for-emergencies/mobile-apps.html.
- Global Health Resources. AAFP. March 22, 2016. Accessed March 21, 2024. https://www.aafp.org/family-physician/patient-care/global-health/resources.html.
- Agarwal A, Crawford N, Nguyen V, Walker A. The White Savior Industrial Complex in Global Health. BMJ Global Health blog. March 11, 2020. Accessed March 21, 2024. https://blogs.bmj.com/bmjgh/2020/03/11/the-white-savior-industrial-complex-in-global-health/.
- Accessed March 21, 2024. https://www.wildmededucationcollaborative.org/.
- National Outdoor Leadership School. Accessed March 21, 2024. https://www.nols.edu/en/wilderness-medicine/resources/.
- The National Conferences on Wilderness Medicine. March 15, 2024. Accessed March 21, 2024. https://wilderness-medicine.com/.
Potential Topics
Wilderness Medicine Components
- Prioritizing in the Wild, and Teamwork with the Non-Medically Trained
- Altitude Illnesses and Management
- Cold Injuries (Hypothermia, Non-Freezing, Frostbite, Immersion)
- Heat Injuries (Hyperthermia, Burns, Sun)
- Trauma/Injuries (Prevention and Pain Management in orthopedic injuries including Podiatry, Airway/Dental, Wound Management)
- Search and Rescue (Litters/Carries, Aeromedical Transport, Water)
- Animals/Insects/Plants (Stings, Bites, Poisonings, Ticks, Snakes, Scorpions, Bears)
- Diving and Marine Medicine (survival at sea, sea creatures)
- Equipment/Special Knowledge (Clothing, Gear, Navigation, Knots/Rope, Protection/Prevention, Surviving the Unexpected Night Out, Water Purification)
- Lightening and Avalanche Injury Prevention and Management
- Care on a Plane (and Other Modes of Transportation)
International Medicine Components
- Basics of Travel Medicine (Preparation, Prevention, Immunizations)
- International Public Health and/or Human Rights (United Nations Human Rights Conventions, Professional Organizations, NGOs, WHO, biostatistics, Epidemiology, Diseases in the Forefront)
- Determinates of Health and Adaptability Serving Internationally (How are health resources distributed. How to find out what those resources are. How to use those resources effectively. Finding out the needs of the community. How to get help/communicate)
- Travelers Diarrhea (Common pathogens, Amebiasis, Cholera, Giardia, Parasites, Food/Water Safety (Including Field Water Disinfection)/Purification, Nutrition, Seafood)
- International Infectious Diseases (TB, HIV, Rabies, Parasites, Ebola)
- Fevers in returned travelers (Typhoid, Dengue, Malaria)
- Tick/Mosquito Borne Diseases/Prevention (Malaria, West Nile Virus)
- Procedures (OB, POCUS, surgery, medical equipment, and medication preparation)
- Cross/Multi-Cultural Medicine, Cultural Competency, Medicine for Refugees and Immigrants (Management of PTSD and psychiatric disorders in survivors of torture, rape and other human rights abuses other mental health concerns like using Critical Incident Stress Debriefing)
- Disaster Medicine: systems of preparedness and application
- Female Genital Mutilation care and other female concerns
- Special populations (children, chronic diseases)
Future Potential WIMP Workshops
- Signal to be found
- Escape and survive a hotel fire
- Obtain food and water
- Survive a plane crash
- Build fires with primitive tools
- Rope skills
- Suturing with low resources
- Splints
- Protect yourself during a disaster
- Assemble & Improvise survival kits
- Construct emergency shelters
- How to safely extricate if trapped in an elevator or other spaces
- Travel safely in developing countries and avoid being “ripped off”
- Blister care
- Orientating such as interpreting topographic (contour) maps, creating/following compass bearing, and applying altimeter / GPS information
- POCUS: Trauma, shock, and undifferentiated hypotension; Pneumothorax, pleural effusion, and pericardial effusion; Abdominal and pelvic pathology; Musculoskeletal injuries; Ocular complaints
Recent WIMP Events
- LifeFlight Lecture
- International Disease Burden of Pneumonia
- Presenting at AAFP
- to WIMP with Stop the Bleed Training
- Lightning Care
- Nepal Trip Lecture
- Presented at FMEC
- Alps Trip Lecture
- Outdoor Wilderness Emergency Care
- International Volunteering Dental Care
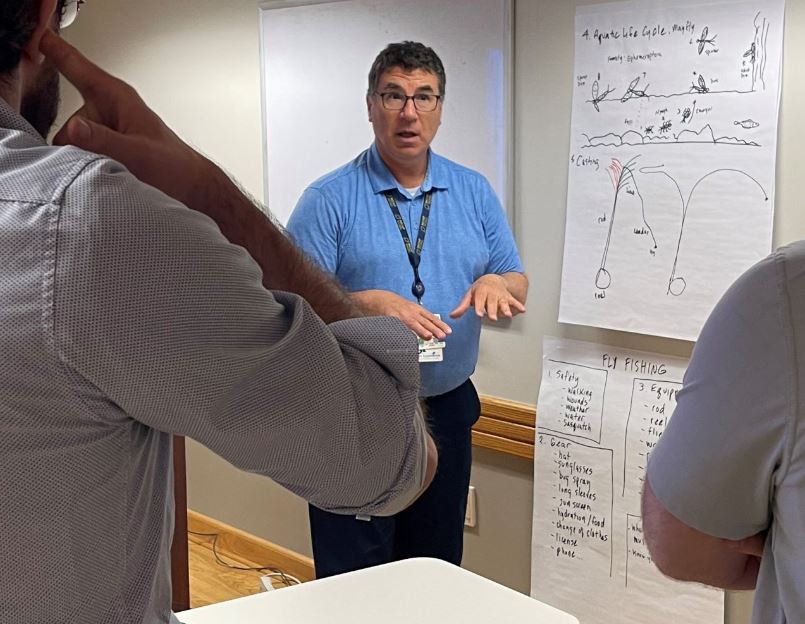
- Fly Fishing
- Camping and White-Water Rafting
- Survival Priorities while walking at Thorncrag Bird Sanctuary
- Treating Bites while at Nightmare on the Ridge
- Movie Night with Trends in International Medicine
- Sledding with Trends in Wilderness Medicine
- African Cuisine and Epipens 201
- International Prenatal Care
- Chili and Survival Structures
- Mountain Medicine on White Mountains Hike
WIMP Photos
Ice Fishing 2025



2024 FMEC

2024 FMEC