On Friday, July 11th, 2025, in Kennedy Park, we hosted our 2nd annual Clinic in the Community in partnership with Healthy Androscoggin and the Maine Family Planning mobile van. It was a great opportunity to make an impact on our friends and neighbors.
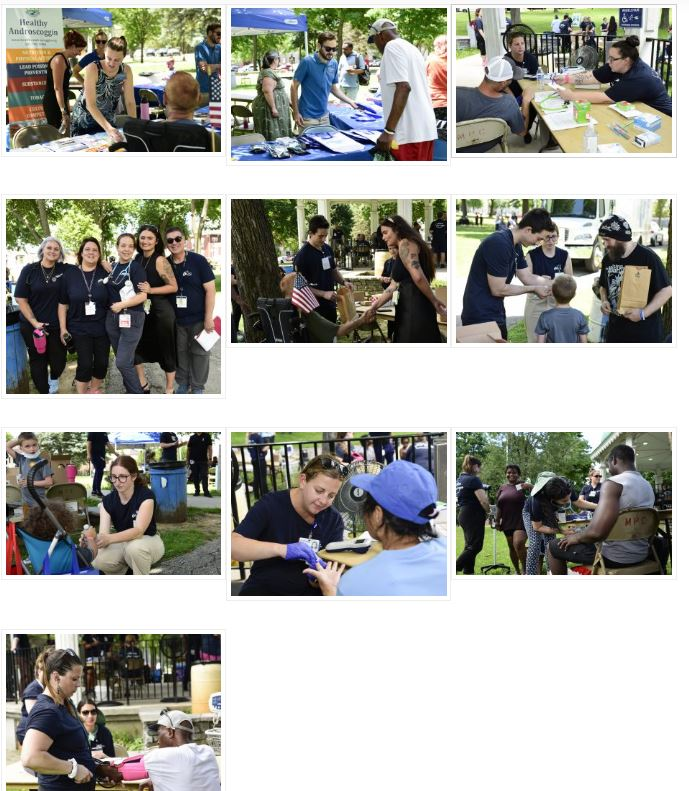
Photos from 2024’s Clinic in the Community