Thank-a-Resident day 2025


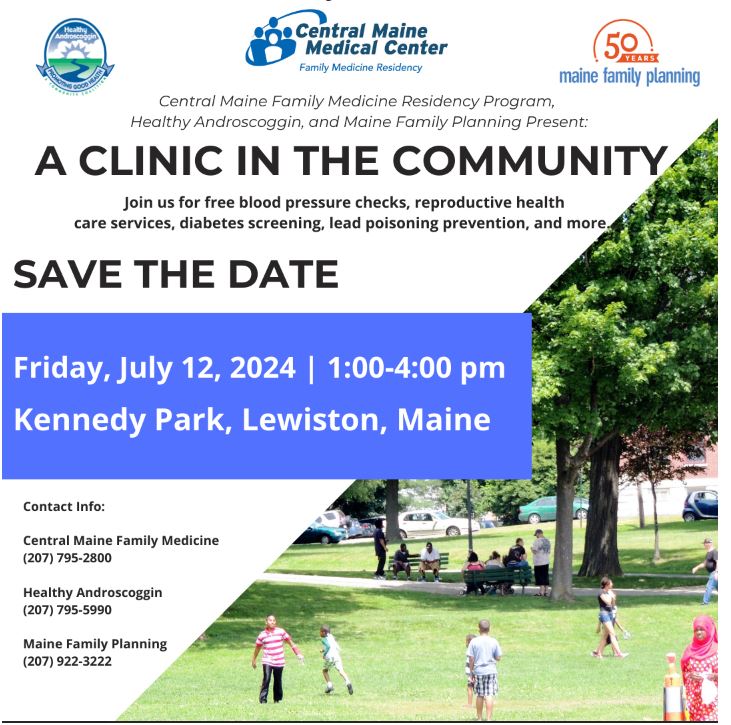
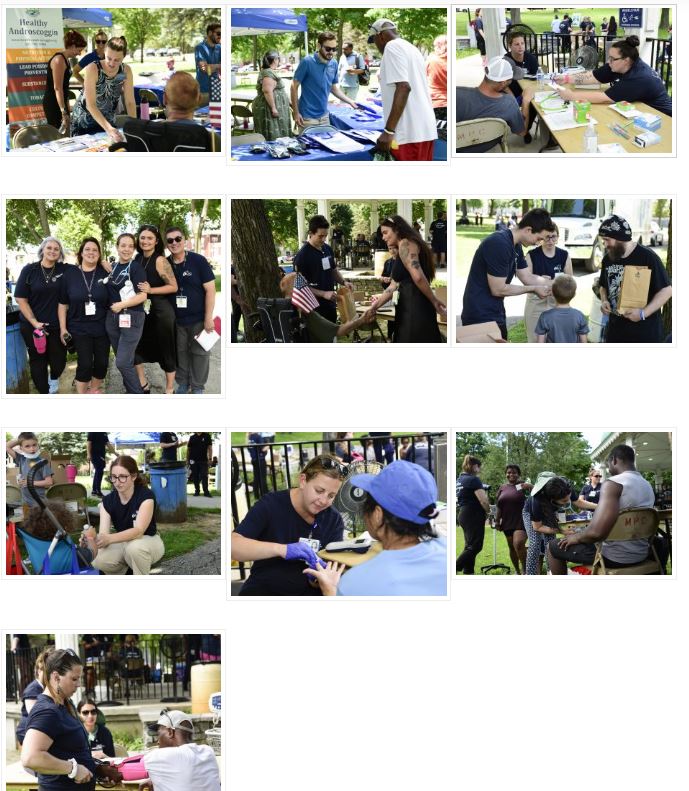
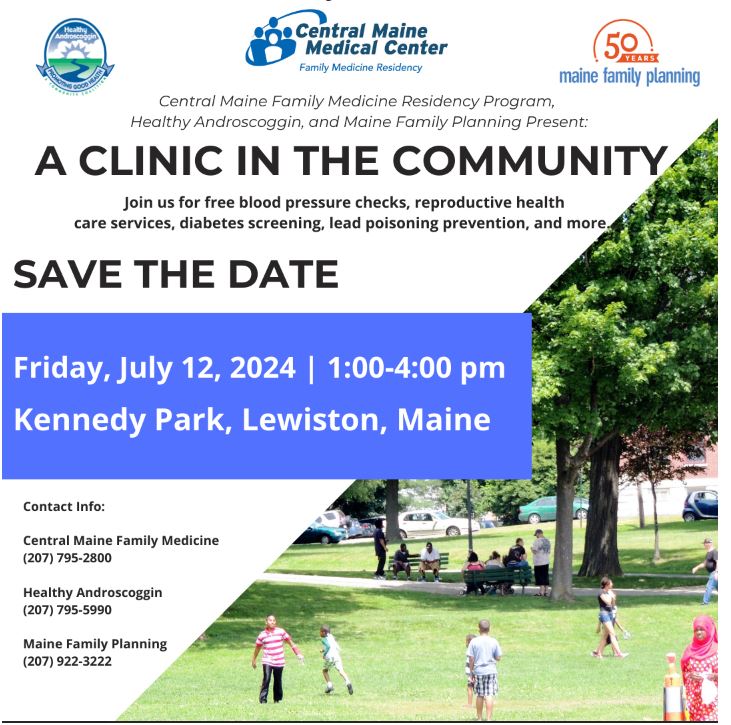
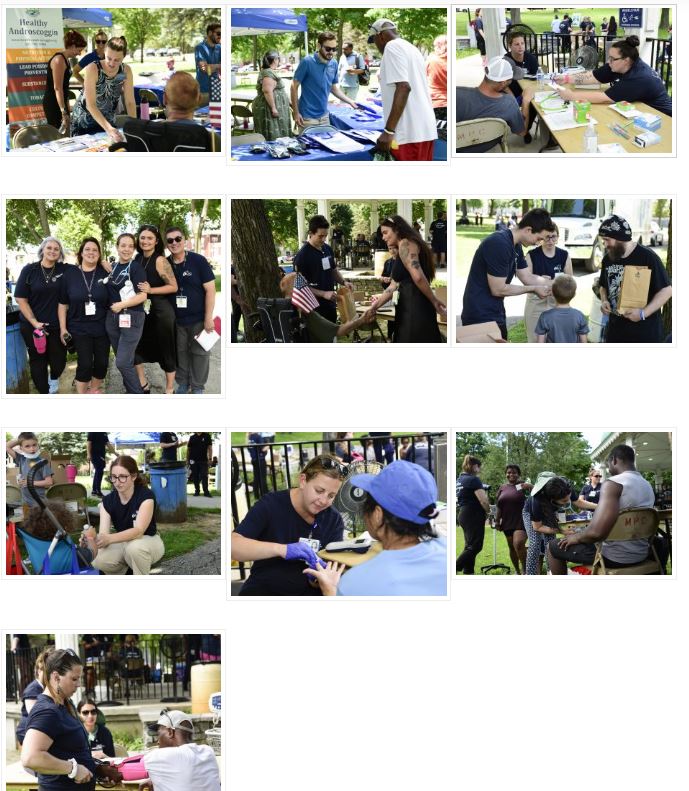
Clinic in the Community
Rally For Recovery


Thank-a-Resident day 2025




CMMC FMR can support residents in most any area of interest, but based on our faculty areas of expertise, current clinical services, and community partnerships, there are some specific strengths of the program that include:
For residents interested in a career in teaching or doing scholarly work, they work on developing those skills and portfolio during residency. Several residents have completed an Academic Medicine elective rotation in the past, which has included partnering with faculty on a research project, spending additional time in our med student clinic, junior precepting, didactic teaching, completing peer-reviews, and presenting at conferences.
We provide a robust MOUD program for patients, and residents participate in all aspects of care including our low barrier bridge clinic and weekly support group as well as managing their own panel of patients on MOUD. For residents who would like additional training in Addiction Medicine, there are opportunities to spend additional time in these clinics, as well as work one-on-one with our Licensed Alcohol and Drug Counselor, who conducts Addiction Assessments of patients in early stages of recovery, and rotate with a community partner for inpatient experience.
Many of our residents have a passion for being agents of change in the community. Advocacy is a powerful way to use your voice as a physician to shape the landscape of health care, particularly at a local level, and residency is a great place to learn those skills. Several residents have completed an advocacy elective that has included speaking at the state legislatures, writing op-eds for the local newspaper, interviewing local and state representatives, researching health policy, and completing advocacy training.
The goal of the Selective is to provide a more compact and comprehensive exposure to the many venues which provide care for the frail elderly: the home, the clinic, assisted living communities, long term care, hospital-based palliative care, and community-based and inpatient Hospice Care. The frail elderly is a fast growing and underserved population which requires a unique set of clinical skills. The goal of this Selective is to help you to be confident and competent caring for elders in your practice after residency.
The Hospitalist in Family Medicine is designed to give residents a concentrated exposure to Hospital Medicine as it evolves into an exclusive area of practice. The resident will work directly with a hospital-based provider group and will participate in the care of patients in that environment. The resident is encouraged to explore all areas in which Hospitalists function which could also include opportunities to rotate in Bridgton or Rumford Hospitals. There may be opportunities to work on the Palliative Care Service as well as serve as a medicine consultant for patients admitted by other providers in the system. This experience may prepare the resident to apply for our or another Hospitalist fellowship.
The goal of the selective is to introduce residents to offering health care through an integrative medicine model. Integrative Medicine combines evidenced-based traditional western or allopathic and osteopathic medicine with other healing traditions, to create an individualized approach for the patient and to support the wellness of the health care provider and team. The resident will gain exposure to a variety of alternative health care providers via an experiential approach and learn to design a holistic method of practice for you and your patients.
Each resident completing the Integrative Medicine selective will also have the opportunity to participate with residents around the nation in the web-based Integrative Medicine in Residency (IMR) program designed by the University of Arizona. IMR is an in-depth competency-based curriculum in integrative medicine to be completed during the second two years of your residency. The IMR incorporates program and topic-specific exercises that residents can incorporate into their day-to-day family medicine experience. Arizona Center for Integrative Medicine
The resident in a sports medicine will have additional training in sports medicine, including opportunities for sideline game coverage, sports medicine research, and increased time in the sports medicine clinic, which allows for increased training in diagnosis and management of musculoskeletal issues. Residents have the opportunity to improve their skills with various procedures including musculoskeletal ultrasound, casting and splinting, joint injections and aspirations, and musculoskeletal x-ray interpretation. After completing this time in sports medicine, the resident should have increased competence at triaging and managing non-operative fractures, tendinopathies and other traumatic injuries, and be comfortable managing non-traumatic musculoskeletal complaints as well.

osteopathicrecognitioninformationbrochure.pdf
Program Goals: Through a variety of innovative curricular experiences integrated throughout the three years of residency (see below), Designated Osteopathic residents in our Family Medicine Program will have a unique and specific set of knowledge and skills with distinct behavioral, philosophical and procedural aspects related to the four tenets of Osteopathic medicine:
This will make you a highly skilled primary care physician capable of approaching patients with in-depth knowledge of Osteopathic Principles and strong skills-based approaches to acute and chronic medical conditions.
Logistics: Prior to entering as a designated Osteopathic resident, applicants should have sufficient exposure to osteopathic philosophy and the techniques of Osteopathic Manipulative Treatment (OMT). Educational background should include, but is not limited to: osteopathic philosophy, history, terminology, and code of ethics; anatomy and physiology related to osteopathic medicine; indications, contraindications, and safety issues associated with the use of OMT; palpatory diagnosis, osteopathic structural examination, and OMT. This could be satisfied by graduating from an Osteopathic Medical School.
If an allopathically trained resident expresses interest in Osteopathic Recognition (OR) they will have access to an equivalent of 200 training hours in Osteopathic Principles and Practice during their three years with us. Acceptance of residents into the ORT will be at the Director of Osteopathic Education’s discretion.
OMM Clinic: Designated Osteopathic Residents will be assigned to OMM clinic every month. Patients will be scheduled for 40 minutes. Initial visit will include history, osteopathic structural exam and appropriate focused physical exam, discussion of treatment plan with the attending physician and treatment with OMT (Osteopathic Manipulative Treatment). Residents are encouraged to treat their patients in continuity clinic. ACGME has requirements on attaining patient encounter numbers we will discuss with you.
Didactic Presentations: Designated Osteopathic Residents will be expected to complete the following:
While on inpatient and subspecialty services, designated Osteopathic residents may be asked to present one or more patients with a complete Osteopathic assessment and treatment plan.
Q. How does the Osteopathic Recognition complement the other required residency rotations? Does this training take the place of other rotations?
A. This is a longitudinal curriculum. Residents learn the additional educational material gradually over all 3 years and the information is integrated into a variety of the core family medicine rotations. Designated Osteopathic residents are given time during selected rotations to learn about additional Osteopathic approaches relevant to primary care. Monthly OMM didactics and semi-annual conferences allow residents to dedicate time to learning hands-on skills from OMM specialists. Designated Osteopathic residents still complete all the same residency rotations as their peers. The goal, first and foremost, is to produce well-trained and highly skilled family physicians; Osteopathic recognition offers the opportunity to apply additional knowledge in OPP and Osteopathic Manipulative Medicine to the benefit of all patients.
Q. What are the educational requirements of Designated Osteopathic Residents?
A. Participate in assigned activities including didactic sessions, noon and quarterly conferences, assigned OMT clinics, didactic presentation assignments, subspecialty clinics and inpatient assignments.
Q. How much time will the program take to complete?
A. The curriculum is longitudinal over 3 years of your family medicine residency. MD residents may need to set aside one of the available PGY2/PGY3 elective months for additional training activities.
Q. How do I apply? Is there a separate match application?
A. There is not a separate match application for this track. Residents interested in pursuing this track follow all the usual residency applications procedures and when you arrange your interview, indicate that you have an interest in hearing more about the Osteopathic Recognition. You will have the opportunity to ask more questions about the track during your interview and can tell us at that time if you’d like to be considered for the track.
Q. Who are the CMMC FMR faculty with training in Osteopathic Medicine?
A. Patricia Collins, D.O.
Paige Picard, D.O.
Christopher Decker, D.O.
Margo Goodman, D.O.
The Family Medicine Residency at Central Maine Medical Center will graduate residents who are:
Central Maine Medical Center (CMMC) commits to creating a collaborative clinical learning environment that fosters ethical and innovative thinking among our physicians in training to provide the skills and resources needed to effectively care for our community.
Given that time is limited during your interview day, below is a list of questions and answers about our residency that we hope will provide helpful information.
| Q | How long has CMMC been training Family Medicine residents? |
|---|---|
| A | Our program began in 1978 |
| Q | Where do your graduates practice Family Medicine? |
| A | Our goal is to train family physicians who are prepared to go to any community and be responsive to local needs, to be leaders, and agents of change wherever they land. However, we always hope they will choose to stay here. Many of our residents do choose to remain in Maine and Northern New England, working in ambulatory primary care and as hospitalists, some go on to fellowships such as Sports Medicine, Geriatrics/Palliative Care, and Addictions Medicine, and some take what they have learned and travel all across the globe to places such as Norway and New Zealand. |
| Q | What does “Clinic First” mean, and how would it influence my education? |
| A | Clinic First is a response to the reality that many family medicine faculty and residents only spend 1-3 half days per week in clinic, which is disruptive to continuity, access, and team-based care—many of the things that bring residents to family medicine in the first place. Residencies that are part of the Clinic First Collaborative make these essential elements of patient care and resident education a priority. At CMMC FMR, we have created a 2×2 block schedule, meaning residents are in clinic for 2 weeks at a time and then on rotation for 2 weeks at a time—no rushing off to clinic for a half day here and there in the midst of a busy rotation schedule. Wherever you are scheduled to be, you can fully immerse yourself in that learning experience. You always know when you will be in clinic, so you can plan ahead for continuity with your patients. |
| Q | What are some highlights of your Family Medicine Center, where I would see my continuity patients? |
| A | We serve a diverse cross-section of the Lewiston-Auburn and surrounding communities that includes elements of both urban and rural low-resourced communities. On any given day, you may see an unsheltered young person, a New Mainer (refugee) who has just arrived in the community, someone living “off the grid” in one of the surrounding rural communities, and an older Mainer, who has lived in the community forever. To meet the needs of our patients, we work as an integrated care team, which includes behavioral health. We provide interprofessional visits, where patients are seen by resident physicians, behavioral health, and pharmacy, for example, and we have monthly teamlet meetings to facilitate communication. Any member of the team can request an interdisciplinary team meeting (IDT) at any time to discuss a patient and develop a shared treatment plan. We also offer home visits that often include both a physician and behavioral health. One area we have been growing over the last few years, in direct response to the needs of our community is Addiction Medicine. We offer a Low Barrier Bridge clinic for OUD and several longer-term treatment pathways. |
| Q | What would my osteopathic education look like if I am a D.O.? |
| A | Our program is accredited under the ACGME with Osteopathic Recognition. All residents will have exposure to and education in osteopathic principles and practice. Osteopathic focused residents, which can include Allopaths, will have additional time practicing OMT in their continuity clinic and on the inpatient service. In addition, we offer osteopathic electives and an OMNN 2 for those looking for opportunities to advance their skills. We have 3 Osteopathic faculty, as well as several community Osteopathic Preceptors to support education and training. |
| Q | Do you have any focus on Resident Wellness as part of your residency program? |
| A | Yes. We have several wellness activities and initiatives including 5th Tuesdays (every 5th Tuesday afternoon the residents have an off-site resident-only gathering), monthly all-staff after work events, a wellness committee (Thrive), and 2 annual resident retreats. However, we believe that true wellness is maintained by residency culture, so we put most of our effort into building and nurturing a culture in our program where residents feel encouraged to bring their whole self to work, where they are supported in staying connected to those parts of themselves that exist outside of medicine, and where they are challenged to reflect on their meaning and purpose, so they grow as much as a person as a physician during their time in the program. |
| Q | What are the academic strengths that will benefit me if I train at CMMC? |
| A | Rigorous hospital medicine training, extensive exposure to Addiction Medicine, ongoing collaboration with a highly skilled Behavioral Health team, OMM, Integrative Medicine, Community-Engaged Learning, and Sports Medicine. Residents are also encouraged to develop autonomy and leadership from Day 1 of residency. They are first responders to Codes; they independently run the hospital service in PGY-2 and oversee interns in PGY-3; they take progressive leadership of their teamlet in clinic; and they are expected to participate in hospital-based committees with support from faculty. |
| Q | What would CMMC FMR offer to me as perks or value-added benefits? |
| A | Full benefits package, complimentary Health and Fitness Center visits including most classes, food stipends when on call, free parking. |
| Q | What is orientation like for new interns? |
| A | Orientation is a month-long experience that includes Continuity Clinic in the FMC; Orientation to the inpatient and outpatient EMR, orientation to the Hospital and the Lewiston-Auburn area; call done with a senior resident; BLS, ACLS and NRP courses with certification; meetings with the Program Director and your Academic Faculty Advocate; a series of new intern noontime didactics and an extensive introduction to competencies and your first rotation. |
| Q | What kinds of connections can I expect to make with the L-A (Lewiston-Auburn) community as a resident? |
| A | You will work in the Dempsey Challenge medical tent, United Way Agency fair, Community Service Day as part of intern orientation, a longitudinal 48-hour community project over the PGY II/III years and give talks in local schools. |
| Q | Can you tell me about the academic appointments and scholarly activities of the CMMC FMR faculty? |
| A | All residents complete a scholarly project, and there are many opportunities to be engaged in other research as well. See the Publications and Presentations section on the website for examples. |
| Q | Will I get to interact with and teach medical students? |
| A | Yes. We have 11 MSIIIs from UNECOM that complete their entire clerkship year in Lewiston. We also have FM clerkship students from Tufts and the University of Vermont and other medical schools. These students will work with you on inpatient and outpatient teams and you will have multiple opportunities to teach and guide their professional development. |
| Q | What is a WIMP? |
| A | The Wilderness and International Medicine Program is a special opportunity available to all residents at CMMC. Please check out our web page for more information. |
| Q | I have some special interests in Family Medicine – will I be able to tailor my education to assure that I gain competency in those areas? |
| A | Yes. We work very hard to individualize the education plan to meet each learner’s needs and desires. We have (An intensive education in a particular area that can include but is not limited to Children/Adolescent Care, Emergency Medicine, Geriatrics/Palliative Care, Inpatient FM Hospitalist, Integrative Medicine (formerly known as CAM), International Health, Maternity Care, Reproductive Health and Wilderness Medicine). We also have ample elective time during which you and your Academic Faculty Advocate can map out a plan to achieve your educational goals. |
As an Intern you would begin residency with 4 weeks of Family and Community Medicine (Orientation). Most blocks are 2×2 – 2 week your continuity clinic and 2 weeks of rotation.
| PGY-1 Rotations | |
| Adult Medicine | 4 Blocks |
| Inpatient Night Float with a senior | 2 Blocks |
| Rural Health | 1 Block |
| OB | 1 Block |
| Pediatrics: Inpatient | 2 Blocks |
| Pediatrics: Outpatient | 1 Block |
| Emergency Medicine | 1 Block |
In your 2nd year, senior residents run the Family Medicine Teaching Service (FMTS) completely independently with the oversight and support of faculty attendings. This will prepare you for your role as the senior overseeing the IMTS in your 3rd year.
| PGY-2 Rotations | |
| Family Medicine Teaching Service (Solo) | 3 Blocks |
| Night Float (Solo and with an Intern) | 2 Blocks |
| OB | 1 Block |
| Pediatrics: Inpatient | 1 Block |
| Sports Medicine | 1 Block |
| Elective 1-4 week block, can be away | 3 Blocks |
In your 3rd year, you’ll oversee Interns on their inpatient medicine rotations.
| PGY-3 Rotations | |
| Inpatient Medicine (IMTS & FMTS) | 2 Blocks |
| Community Engaged Learning | Longitudinal |
| Inpatient Night Float (Solo and with an Intern) | 2 Blocks |
| ICU | 1 Block |
| Pediatrics: Outpatient | 1 Block |
| Sports Medicine | 1 Block |
| Elective 1 4-week block can be away | 3 Blocks |
5th Tuesday Wellness Activities
Behavioral Health
Grand Rounds
Home Visits
M&M
Monthly Teamlet Meetings
MOUD
Nursing Home and Long-Term Care
Practice Management and Population Health
Resident Lectures
Scholarly Activity
Weekly Didactics
Academic Year 2026-2027 *Stipend amounts Beginning July 1st, 2026
| Annual Stipends* | PGY1 | $71,438 |
| PGY2 | $74,837 | |
| PGY3 | $77,951 | |
| Choice Time Off (CTO) | 22 Days | |
| Other Paid Time Off | Includes: Extended Sick Bank, Bereavement, Family Leave, Jury Duty, Adoption Assistance | See CMH Specific Policy |
| Meal Account | $1,600 per year | |
| Certification | Residency sponsored and tuition paid for: CLS, PALS, ALSO, NRP | |
| Licensure | Up to $1000 (one time) associated expenses | |
| Board Certifications | Reimbursement costs for ABFM/ABOFP Board Certification Exams taken during residency (per FMR policy) Reimbursement cost for USMLE or COMLEX Step 3 | |
| Memberships | AAFP for all residents; AOA for all Osteopathic residents | |
| CME | $1800 total for 3 years | |
| Malpractice | Claims made for services provided while under contract | |
| Retirement Account | TSA-403B | |
| Voluntary Benefits | Benefits include: Insurance with family coverage available (no pre-existing clause), dental, life, long term disability, healthcare spending account, dependent care spending account. | Residents chooses how to spend dollars allotted by CMMC. |
| Moving Expense for matched applicant | One time; must submit receipts | Up to $1000 |
| The Y at CMMC Wellness Center | The facility offers an assortment of cardiovascular and strength equipment, well equipped locker rooms, personal trainer services and a variety of facilitated exercise classes. | Membership is paid. |
| Team Building | Bi-annual retreats for residents; annual outing with faculty, 5th Tuesdays, community service. THRIVE |
Shari Casiano Vega, MD – Looking for her next adventure in Maine
Jas Gill, MD – Primary Care, Vancouver, British Columbia
Emily Hill, DO – Maine Medical Center, Hospice & Palliative Care Fellowship, Portland, ME
Taz Noori, MD – Hospital Medicine, Nova Scotia, Halifax
Saraja Pandit, MD – Primary Care, Beth Israel – Lahey, Peabody, MA
Jack Ritzo, MD – Medical Office of John A. Ritzo, MD, San Mateo, CA
Travis Frazier, MD – Osteopathic Neuromuscular Medicine
Fellowship, Maine-Dartmouth, Augusta, ME
Mankaran Gill, MD – Family Medicine, Greater Toronto Area,
Canada
Kelsey Hickey, DO – Hospitalist Fellowship, CMMC, Lewiston,
ME
Celeste Hutton, MD – Family Medicine Practice, Lewiston, ME
Jaclyn Israel, DO – Redington Fairview General Hospital Family Medicine, Skowhegan, ME
Luke Ollila, DO – Family Medicine, Greater Portland Area, ME
Ruby Singh, MD – Revolutionary on sabbatical, brainstorming non-corporate paths to happiness
Residency Graduates 2023
Colin Bonnar, MD – Primary Care at Nova Scotia Health Authority, Baddeck, NS
Eliza Foster, DO – VA Togus, ME
Matthew Levasseur, DO – Addiction Medicine, Federally Qualified Health Care, Austin, TX
Anna Levit, MD – Integrative Medicine Educator Fellowship, Cambridge Health
Alliance, Malden, MD
Catherine Lok, DO – Founder and Physician, RiverRock Clinic, Woodfin, NC
Emily Nguyen, MD – Travel/Locum work, British Columbia, Canada
James Poulin, MD – St. Mary’s Orthopedic
Matthew Rausch, DO – Family Medicine/Primary Care, Family Health
Associates, Auburn, ME
Residency Graduates 2022
Jeffrey S. Badillo, MD – Northern Light Health Primary Care, Yarmouth, ME
Christopher M. Caracciolo, MD, MPH – Primary Care, Coos County Family
Medical Center, Berlin, NH & Hospitalist, Androscoggin Valley Hospital, Berlin,
NH
Ian J. Corbett, DO – Topsham Family Medicine, Topsham, ME
Cecilia V. Davies, MD – Intermountain Healthcare, Riverton, UT
Dana E. Kennedy, MD – Lamoille Health Family Medicine, Morrisville, VT
Anthony M. Pastore, DO – Northern Light Mercy Primary Care, Windham, ME
Isabella C. Taylor, DO – Lisbon Family Practice, Lisbon, ME
Residency Graduates 2021
Charles Bergeron Poulin MD – Central Maine Healthcare, Naples, ME
Patricia Collins DO – Central Maine Healthcare, Lewiston, ME
John Cooper III DO – MaineGeneral Medical Center, Augusta, ME
Kevin DeGroot DO – Mercy Health, Vermilion, OH
Myriam Jolicoeur MD – Central Maine Healthcare, Naples, ME
Jessica Lucas DO – DownEast Orthopedics, Banger, ME
Marie-Alexandria Tremis MD – Central Maine Healthcare, Lewiston, ME
Residency Graduates 2020
Jennifer Couture DO
Christopher Decker DO
Justin Quinlan DO
Olivian Simpson MD
Bryan Stanley MD
Ross Watson MD
Terra Wilkins MD
Residency Graduates 2019
Navneet Garcha MD
Bindu Gupta MD
Jennifer Hanson MD
Christine Lincoln DO
Scott Lowman DO
Kathryn McLellan MD
Samuel Moss DO
Residency Graduates 2018
Colette Charles MD
James Flannery MD
John Gunel DO
Sarah Kelley-Spearing DO
Susan Miller MD
Ankur Patel MD
Residency Graduates 2017
Clare Alexander MD
Tony Chan MD
Benjamin Kamin MD
Frank “Zach” Mazone II DO
Nupur Nagrare MD
Shayna Shackford DO
Residency Graduates 2016
Nicole Boutaugh DO
Leslie Bradbury MD
Kara Callahan MD
Joshua Garfein DO
Sean Tyler O’Sullivan DO
Gregory Thibodeau MD
Lisa Torgersen MD
Residency Graduates 2015
Clayton Bell MD
Aaron Hoffman DO MPH
Genesis Juat MD
Erik “Seth” Kramer DO MPH
Mariette Macrander MD
Aliya Rahemtulla MD
Margo Sullivan Goodman DO
Residency Graduates 2014
Catherine Krouse DO
John Lowery DO PhD
Jaime Nemeth DO
Joanie Peter MD
Preethi Rajanna MD
Marc Seeley DO
Sandhya Tagaram MD
Residency Graduates 2013
Adam Duquette DO
Emily Fontaine MD
Michael Johns MD
Christopher “Todd” Kitchens DO
Shayna Lemke DO
Gonzalo Ruiz MD
Residency Graduates 2012
Stephanie Aung MD
Harpreet Ghotra MD
Swapna Gummadi MD
Petrona Manasseh MD
Huy Nguyen MD
Annamarie Pond DO
Ravi Sathya MD
Residency Graduates 2011
Shaik Basha MD
Alicia Koteles MD
Brad Long MD
Jeffrey Lynds MD
Lisa McAllister DO
Rhianna Meadows DO
Stephanie Youd Sinclair MD
Residency Graduates 2010
Stephen Adams MD
Neelima Ganta MD
Jennifer Dressel MD
Michael Gravatt MD
Bina Maharjan MD
Laurel Schwingel DO
Terry Ann Scriven MD
Residency Graduates 2009
Brian Dressel MD
Shauna McElrath DO
Carlos Martinez MD
Patrick Pine MD
Sumathi Rajanna MD
Gary Rivard DO
Residency Graduates 2008
Trevor Braden MD
Vasuki Nagaraj MD
Jesse Reynolds MD
Christine Swartz MD
Thom Tigley MD
Residency Graduates 2007
Christopher Cieurzo MD
Manju Hilary MD
Stephen Kulcsar DO
Kirk Silver MD
Christine Tremblay DO
Residency Graduates 2006
Balint Budai MD
Magili Chapman Quinn DO
Michael Kaylor MD
Narayana Padala MD
Nathan Raby DO
Geniene Wilson MD
Residency Graduates 2005
Timothy Burdick MD
Cortney Linville DO
Joseph Martinez MD
Margarita Perchonok Shugol DO
Stacey Walden DO
Residency Graduates 2004
Shannon Kenney DO
Peter Kulawiec MD
James Ostrander DO
Karen Roberts DO
Ira Robles MD
Flora Sadri-Azarbayejani DO
Residency Graduates 2003
Michael Bell MD
Veena Channamsetty MD
Sandra Corbett DO
Jennifer Nelson DO
Brian Newman DO
April Shelton MD
Residency Graduates 2002
Jeff Cote MD
Angelisa Janssen MD
Gerry Lachance DO
Nidal Morrar MD
Jennifer Ryan DO
Residency Graduates 2001
Denise Arcand MD
Jill Herr MD
Rebecca Canner MD
Patrick Keith MD
Beth Lakd MD
Sarah Skelton MD
Jim Stephenson
Residency Graduates 2000
Marc Daigle MD
Denise Frigon Cogle DO
Nathan Murray-James MD
Henry Youga MD
Residency Graduates 1999
Paul Benson MD
Diane MacKinnon MD
Dewayne Niebur MD
Molly Rossignol DO
Linda Youngren MD
Residency Graduates 1998
Emily Ferguson MD
Paula Greenleaf DO
Diana Kistler DO
Susan Lemei MD
Elizabeth Pierce DO
Residency Graduates 1997
Thomas “Tom” Bosma MD
Shannon Deschenes DO
Trisha Gushue DO
Ray Tardif MD
Residency Graduates 1996
Mary “Mer” Ashmore DO
Diane Eodice DO
Deboarh Learson MD
Stephen Molnar-Gabor MD
Martha Stewart DO
Residency Graduates 1995
Julia Crawford MD
Paul Davis MD
Jonathan Nwanagu MD
Wendy Weiss DO
Residency Graduates 1994
Arthur “Art” Manning DO
Thanh Bui MD
Residency Graduates 1993
Peter Beeckel MD
Mark Roterson MD
Paul Podett MD
Brigitte Engelhardt MD
Kristy Murray-Pulsifer DO
Residency Graduates 1992
James “Jim” Linnick DO
Marilyn Assistores MD
Savita Joshi MD
Sarah Prescott DO
Lynne Senty DO
Teresa Klyzejko MD
Residency Graduates 1990
Bradley Anderson MD
Sharon Curtis MD
Steven Dickter MD
Samual “Sam” Hunkler MD
Residency Graduates 1989
Scott Chaffin DO
Lisa Kowalski MD
Brian Smith MD
Diane Zavotsky MD
Residency Graduates 1988
Stephen Fairchild MD
Linda Moorhead MD
Cynthia Strout MD
Residency Graduates 1987
Margaret “Peggy” Matthews MD
Kurt Oswald MD
Jeffrey Palmer MD
Fred van Mourik MD
Residency Graduates 1986
Frederick “Fred” Gleeson MD
Jay Kaminski MD
Jeffrey Martin MD
Residency Graduates 1985
Jay Burns MD
Charles “Chuck” Judy MD
James Kilgour MD
Diane Pittman MD
Residency Graduates 1984
Hans Duvefelt MD
Daniel “Dan” Mingle MD
Denise Winings MD
Residency Graduates 1983
Greg Bowerman MD
Karen Young MD
Residency Graduates 1982
Robert “Bob” Abramsen MD
Richard Gilliam MD
David Kristensen MD
Patricia Parsley MD
Residency Graduates 1981
Theodore “Ted” Brooks MD
Lawrence Feld MD
M. David Lauter MD
Patricia Williams MD
Residency Graduates 1980
Bruce Alexander MD
Stuart Andrews MD
Charles Burns MD
William “Billy” Leach MD
The Gerrish-True Health Sciences Library at Central Maine Medical Center offers dozens of links to websites that offer accurate medical and health information. It is a resource available to patients, the public and to medical staff.
Gerrish-True Health Sciences Library
Central Maine Medical Center
300 Main Street, P.O. Box 4500
Lewiston, ME 04240
Library Hours:
Public Access: Monday – Thursday 8 a.m. – 4 p.m., Friday 8 a.m. – 3:30 p.m.
Hospital clinicians and team members: 24/7 access with badge
Librarian on-site as needed and by appointment
Library Staff:
Sarah Hudson, MLS, MBA call: 207-795-5956 or email: hudsonsa@cmhc.org
For more information call: 207-795-2560 or email: library@cmhc.org
Collections and Services: The Gerrish-True Health Sciences Library supports the health-related information needs of physicians, hospital team members and all affiliated students. Patients, their families and the public are welcome to use the library during staffed hours.
The Gerrish-True Health Sciences Library subscribes to medical and health-related journals. The majority of these are available online through our medical databases (see Professional Health Resources). CMH medical staff and students may contact the CMMC Library team members for online access instructions. Journals are indexed in PubMed with links out to the full text of journals in electronic format. Older issues may be available in storage or on microfilm. Print journals do not circulate but may be photocopied. (Photocopying is available.)
The library has a small print collection of medical reference books arranged by National Library of Medicine classification in many specialty areas. Check the CMMC online catalog for availability. Books in the circulating collection may be borrowed for two weeks and may be renewed. Electronic textbooks are also available through Nursing and Access Medicine on the Professional Health page.
Health Library Disclaimer: Please note: Information provided by the Gerrish-True Health Sciences Library or links on its web page, is not intended to be a substitute for medical advice or care from a physician of other healthcare provider. Please call your healthcare provider if you have questions regarding your specific medical condition.
Medlineplus – MedlinePlus is the National Institutes of Health’s Web site for patients and their families and friends. Produced by the National Library of Medicine, it brings you information about diseases, conditions, and wellness issues in language you can understand. MedlinePlus offers reliable, up-to-date health information, anytime, anywhere, for free.
CDC – CDC (Centers for Disease Control and Prevention) works 24/7 to protect America from health, safety and security threats, both foreign and in the U.S. Whether diseases start at home or abroad, are chronic or acute, curable or preventable, human error or deliberate attack, CDC fights disease and supports communities and citizens to do the same.
ConsumerMedSafety – Developed by the Institute for Safe Medication Practices (ISMP), ConsumerMedSafety.org is designed exclusively to bring the message of medication error prevention directly to the consumers. Features of the site include:
Druginfonet.com – Official package inserts and pharmaceutical product and disease information for healthcare professionals and consumers.
Family Doctor.org – The Family Doctor website is operated by the American Academy of Family Physicians (AAFP), a national medical organization representing more than 115,900 family physicians, family practice residents and medical students. All of the information on this site has been written and reviewed by physicians and patient education professionals at the AAFP.
US Food and Drug Administration
Healthfinder.gov – A gateway to reliable consumer health and human services information, sponsored by the DHHS.
Household Products Database – Information on the health effects of common household products under your sink, in the garage, in the bathroom and on the laundry room shelf.
KidsHealth.org – Doctor-approved health information about children, created by the Nemours Foundation.
Lab Test Online – Lab Tests Online has been designed to help you, as a patient or family caregiver, to better understand the many clinical lab tests that are part of routine care as well as diagnosis and treatment of a broad range of conditions and diseases. If you are a medical professional, this site can serve as a quick reference tool or as a resource for keeping up with advances in laboratory science.
Marvel – Free Maine databases including Academic Search Premiere, Business Source Premiere, Health Source: Consumer Edition, Proquest Newspaper Indexes
Mayo Clinic – Consumer website offering health and medical information and disease management, produced by the Mayo Foundation.
Nutrition.gov – A U.S. federal guide offering access to all government web sites with reliable and accurate information on nutrition and dietary guidance.
President’s Council on Fitness, Sports & Nutrition – The President’s Council on Fitness, Sports and Nutrition mission is to engage, educate, and empower all Americans across the lifespan to adopt a healthy lifestyle that includes regular physical activity and good nutrition.
RxList – RxList is an online medical resource dedicated to offering detailed and current pharmaceutical information on brand and generic drugs. Founded by pharmacists in 1995, and acquired by WebMD in 2004, RxList is continuously reviewed and updated with articles written by pharmacists and physicians and data provided by credible and reliable sources like the FDA, Cerner Multum, and First Data Bank, Inc. to ensure the most accurate and beneficial information is provided.
NIH Senior Health – Health and wellness information for older adults from the National Institutes of Health.
NIH Tox Town – An interactive guide about how the environment, chemicals and toxic substances affect human health.
USDA ChooseMyPlate.gov – The Center for Nutrition Policy and Promotion lists the Dietary Guidelines for Americans, the USDA Food Guidance System, the Healthy Eating Index, and many other nutrition resources on Choose My Plate including U.S. Meal Plans.
Womenshealth.gov – The FDA’s leading resource for women’s health information.
State and Local:
State of Maine – Home page for links to Govenor’s office, State Agencies, Quasi-independent Agencies, Legislature (statutes, bills, House, Senate etc.).
Maine State Library – Home page for the Maine State Library and additional reference databases.
News:
USA Today
Lewiston Sun Journal
Portland Press Herald
The following databases are available for medical staff and students. Please contact the library to obtain access information.
Medical Databases
Nursing and Allied Health Databases
Team Member Remote Access – remote access your CMH desktop from any computer
Outlook Web Access – remote access to check your Outlook email from any computer
iCare – HealthStream Learning Center – access to your iCare assignments and online education
Team Member Benefits & Wellness Information – CMH Benefits and Wellness information
Lab Help – Laboratory test information
Our nurses embody this mission by following a Nursing Practice model focused on relationship-based care, ensuring that patients and family are at the center of all we do. By nurturing communication between healthcare teams and with our patients and their families, our nurses strive for caring conversations that help anticipate each individual’s needs.
In order to create a nurturing environment, the vision of our Nursing Department is to employ passionate, professional nurses who provide high-quality holistic care to our patients. We believe that the practice of holistic nursing promotes an environment for optimal well-being of the body, mind and spirit.
We combine our vision to employ passionate and professional nurses with our philosophy of professional excellence by evolving the creative art and science of nursing. Patients are treated as members of our own families, with a focus on dignity, respect and what matters to them. We include our patients and their family members in all aspects of decision-making in order to provide what matters most — at the time it matters most.
CMH nurses fulfill many roles within their patient’s care team besides providing direct patient care. They often serve as educators, interpreters and advocates for our patients. This includes helping our patients and their families understand the health issues they’re facing and the potential resources available to them, while serving as their advocate in order to promote the best possible outcome for each patient.
At Central Maine Healthcare, our nurses are more than a team of skilled, dedicated professionals. We are also a close-knit community of friends and neighbors who support each other in the pursuit of a common goal: providing exceptional, evidence-based care that puts patients at the center of everything we do.
Ours is a diverse community of nurses with a wide range of degrees, specialty training and certifications, and that diversity is our strength. We use each nurse’s unique skills and talents to achieve our vision of a team of passionate, professional nurses providing high-quality, holistic care that matters to our patients. We foster a safe patient- and family-centered experience that is open and responsive to the communities we serve.
As nurses, caring for patients in times of illness or injury is only part of our role. We’re also educators and advocates. We provide education to empower people to achieve their health and wellness goals, and we champion their efforts by providing support, guidance and connections to helpful resources. Our philosophy reflects the marriage of art and science in the multidimensional role nurses play at CMH: We, as a nursing community, assure professional excellence by evolving the creative art and science of nursing. Patients are treated as if they are members of our own families, focusing on dignity, respect and what matters to them.
We foster a respectful, supportive environment in which every nurse feels empowered to achieve their personal and professional best. Our nursing community embraces:
The CMH practice model exemplifies a culture that empowers and supports nurses to advance their professional development from Novice to Expert. This means helping them stay on top of the ever-changing healthcare industry through our Professional Advancement Program, TeamSTEPPS program and other career opportunities. By focusing on their professional growth, our nurses learn how to make positive changes that directly impact our patients.
By making this investment in our nursing team members, we hope to show them how appreciated they are for the specialized contribution they make every day in the delivery of healthcare and their ability to positively affect care and outcomes of our patients. We believe this is essential to provide the highest quality care to our patients in today’s healthcare environment.
Feeling inspired to give back to your community? Consider a career in nursing at Central Maine Healthcare. We are always looking for talented, compassionate nursing professionals to join our team, and you may be the perfect fit. Let us know you are interested by applying online, and one of our recruiters will get back to you with details.
Contact our human resources department at 207-795-2392 or recruitment@cmhc.org.
In 2009, Central Maine Hospitalists (CMH), in collaboration with Central Maine Family Medicine Residency (CMFMR), began offering a one-year fellowship for a family medicine or internal medicine graduate interested in pursuing a career as a hospitalist. Based on our highly successful initial experience with this program, in 2012 we expanded the program to include up to two fellows per academic year. We hope you will contact us if you are interested in focusing your career on inpatient medicine.
CMH was established with five experienced physicians in 2004 and has now grown to over thirty board-certified physicians and associate professional staff (NP/PA). We care for over 50% of the inpatient population at Central Maine Medical Center (CMMC), a 250-bed community teaching hospital as well as provide care at our affiliated critical access hospitals. All members of CMH are actively involved in a number of hospital processes including: division and group leadership, quality improvement, guideline development and implementation, patient safety, medical education, palliative care and information technology. We are also involved in the Society of Hospital Medicine (SHM), including Fellows and Senior Fellows of Hospital Medicine. Several of our members have earned a Recognition of Focused Practice in Hospital Medicine (RFPHM). Our group members have been active in and presented at SHM local chapter meetings, as well as national SHM forum leadership, committee membership and leadership. All members of the group are committed teachers involved in educating the hospitalist fellows, residents, medical and pharmacy students.
CMFMR has been educating family physicians since 1978. We provide care and training to diverse populations and our graduates are regularly hired into the hospital system. The opportunity to partner with the hospitalist group builds on our reputation for excellent inpatient training and our flexibility in establishing programs to meet student and resident needs. The department of family medicine has established a reputation for advanced thinking in organizing for the provision of care and has become a research setting for the rest of the outpatient practices at CMMC. Modeling excellence in interdepartmental cooperation, CMH and CMFMR are exceptionally well-suited to educating Hospitalists Trained in Family Medicine (HTFM).
Dr. Geyer and our program were recently featured in The Hospitalist, August 2019: “We rely heavily on the Core Competencies in Hospital Medicine developed by SHM, which emphasize clinical conditions, medical procedures, and health care systems. Gaining fluency in the latter is really what makes hospital medicine unique,” Dr. Geyer said. “Often residency graduates seeking work in hospital medicine are insufficiently prepared for hospital billing and coding, enacting safe transitions of care, providing palliative care, and understanding how to impact their health care systems for quality improvement, patient safety and the like,” she added.
Dr. Geyer said his fellowship does not mean just being a poorly paid hospitalist for a year. “The fellows are clearly trainees, getting the full benefit of our supervision and supplemental training focused on enhanced clinical and procedural exposure, but also on academics, quality improvement, leadership, and efficiency,” she said. “All of our fellows join SHM, go to the Annual Conference, propose case studies, do longitudinal quality or safety projects, and learn the other aspects of hospital medicine not well-taught in residency. We train them to be highly functional hospitalists right out of the gate.”
