Mental Health Program for Older Adults
Your mental health matters, especially as you get older. That’s why Bridgton Hospital provides Senior Life Solutions, outpatient services designed to meet the unique needs of older adults experiencing depression, anxiety, or other mental challenges often associated with aging.
More than 20% of people over the age of 55 experience some type of mental health concern, yet more than half of those people receive no treatment. Studies show that over 50% of older adults believe it’s normal to get depressed as they age. It’s not! Feeling down every once in a while is a normal part of life, but if these feelings last weeks or months, you may be dealing with something more serious.
Get more information about Bridgton Hospital’s Senior Life Solutions program by calling (207) 647-6272. Anyone can make a referral.
What is Senior Life Solutions?
Senior Life Solutions helps older adults who are experiencing a mental health challenge develop the coping and communication skills they need to live a healthier and happier life. Our clinical team includes a board-certified psychiatrist, licensed therapists, a registered nurse, and other professionals dedicated to the mental health care of the older adults in our community. We help ensure you get an accurate diagnosis and appropriate treatment to significantly reduce symptoms of depression and anxiety.
Our group therapy sessions are held up to three times a week at Bridgton Hospital. Participants may have the option to attend these sessions virtually, using a computer, tablet or smartphone connected to the internet. We also set aside time for individual psychotherapy and check each on-site participant’s vitals.
Services offered by Bridgton Hospital’s Senior Life Solutions include:
- confidential, comprehensive assessment
- individual therapy
- group therapy
- family therapy
- medication education and management
- after-care planning
Even though this is a group setting, each person is addressed individually based on their unique needs. We continue to engage and support our participants after they complete the program.
Who Can Benefit from Senior Life Solutions?
Our program is designed to help people typically 65 and older who are experiencing symptoms of depression, anxiety, and other mental health challenges, including suicidal thoughts and intense grief.
If you or someone you know has experienced any of the following, this hospital-based outpatient program might be right for you.
- Anxiety
- Changes in appetite
- Depression
- Difficulty sleeping
- Feelings of sadness or grief lasting more than two weeks
- Feelings of worthlessness or hopelessness
- Lost a spouse or close family member
- Loss of energy
- Loss of interest in previously enjoyed activities
- Recently experienced a traumatic event
Anyone can make a referral to the program. This includes self, family members, physicians, or other healthcare professionals.
For more information about Bridgton Hospital’s Senior Life Solutions program, call (207) 647-3272. Our program is located at Bridgton Hospital, 25 Hospital Drive, Bridgton, Maine.
Senior Life Solutions Outcomes
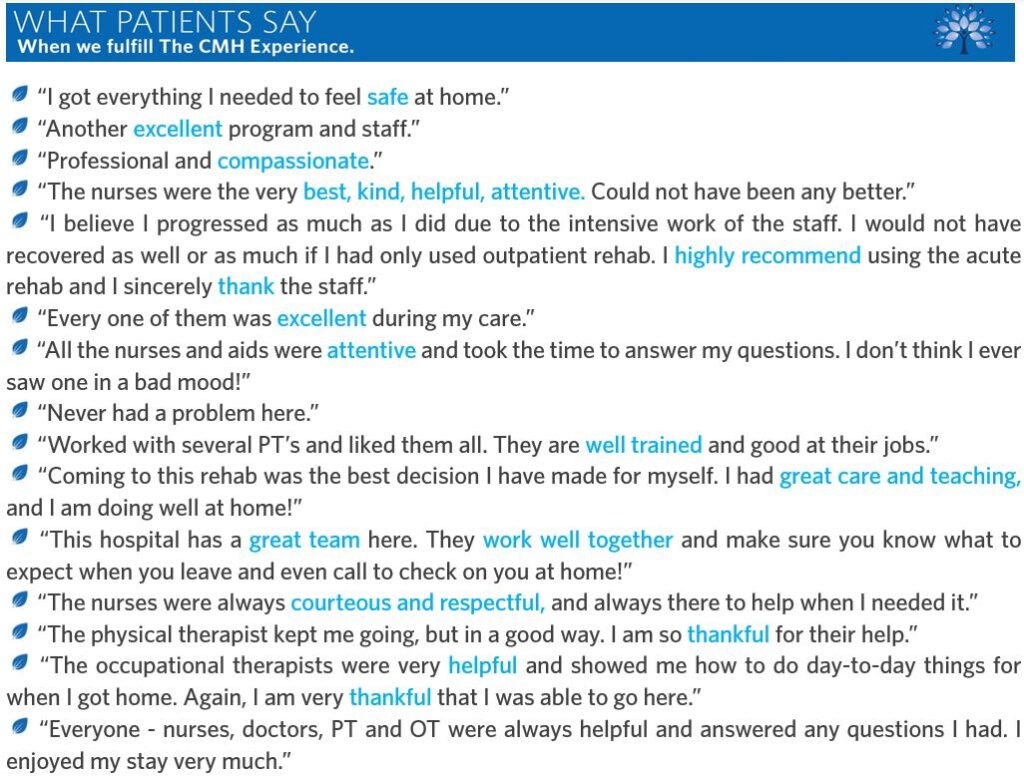
Over 90% of our program participants report a significant improvement in symptoms.
The majority of participants who complete our outpatient program score well below the threshold for depression and anxiety on standardized measurement scales.
Our team monitors your progress throughout the program, including your physical health. Many participants experience improvements in their physical health by reducing stress and symptoms of mental health challenges.
Our Approach
Empowerment Through Connection
Loneliness and isolation can take a toll on mental health. Our program promotes a sense of belonging and community. We offer group sessions, peer support, and activities that foster social bonds, helping older adults feel more connected to others and to life itself.
Mindful Wellness
We emphasize the importance of self-care, mindfulness, and stress management. Through mindfulness exercises, relaxation techniques, and cognitive-behavioral strategies, we help older adults reduce anxiety, depression, and age-related stressors.
Personalized Support
Every individual’s journey to mental well-being is unique. Our experienced team develops personalized care plans for each program participant. These plans address their specific needs and goals, ensuring that they receive the right support at the right time.
Why Choose Senior Life Solutions?
Experienced Team: Our compassionate and highly skilled team specializes in geriatric mental health and is dedicated to improving the lives of older adults.
Proven Results: We have a track record of helping older adults achieve better mental health, leading to increased happiness and overall well-being.
Safe and Inclusive Environment: We prioritize creating a safe and inclusive space for seniors of all backgrounds and experiences.
Community: Be part of a community that values your journey and supports your mental health every step of the way.
Join Us Today
Take the first step toward better mental health and emotional well-being. Senior Life Solutions guides you on a path to a happier, healthier, and more fulfilled life. Contact us today to learn more about our mental health program for older adults and how you can get involved.
Remember, it’s never too late to prioritize your mental health and find the support you deserve. At Bridgton Hospital, we’re here to help you thrive in your golden years.